By: Dr. Alan Christianson
By: Dr. Alan Christianson
Fatty
liver is expected to become the top cause of liver transplants in the
next decade. It’s difficult NOT to see fatty liver disease as one of the
most pressing healthcare issues in this country. [1, 2] The good news
is it is very reversible.
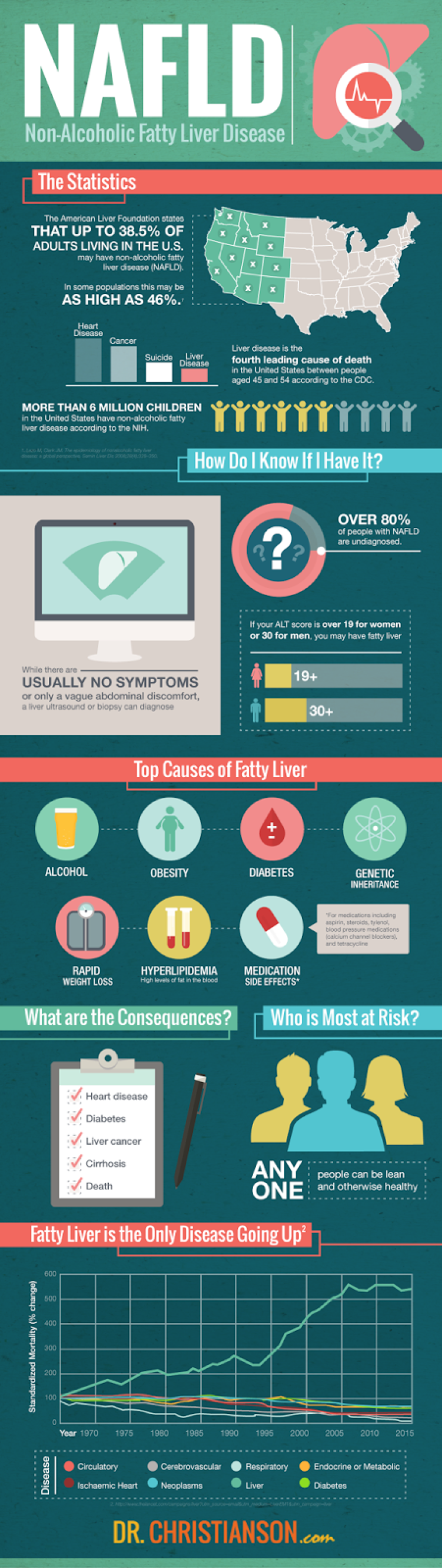
Shocking Stats
Liver
disease is the fourth leading cause of death in the United States among
45-54 year olds and, sadly, affects more than 6 million children. As
childhood obesity has gone up, researchers are expecting it to cause
more complications in kids in coming years.
One problem is that it
is hard to diagnose. While we can easily measure things like blood
sugar or iron levels, the perfect way to find out if a liver is diseased
would be to take it out and analyze it. Liver biopsies are the most
accurate way to diagnose fatty liver, but they are not at all practical
as screening tools.
When researchers examined 70 such biopsies from
healthy
relatives hoping to donate liver tissue to a loved one who needed a
liver transplant, they found 38.5% of the healthy relatives had fatty
liver disease. Another study found that elderly individuals who were
hospitalized for
non-liver causes had a 46% chance of having
fatty liver disease. If that’s not enough, the rates of fatty liver in
obese populations may be as high as 90%. [3]
 What is it?
What is it?
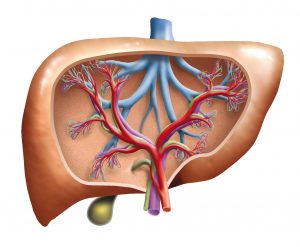
Fatty
liver is a sign that the body is not burning its fuel right. When you
eat, your body breaks food down into fuel which either gets burned or
stored as body fat. When you’re energized, you’re active and alert.
Movement is effortless and life is good. On the other hand, the more fat
your body stores, the more you’re growing stuff you probably don’t want
to grow and the more you’re just running down, feeling far from your
best. When you store more, you’re more apt to have more fats, especially
triglycerides, get stuck in your liver and enlarge it. A healthy liver
has about 1-3% fat. Once you get over 5% things start to go wrong. Once
you get over 10%, disease usually sets in. All this fat can lead to
problems like a poorly functioning liver, liver tissue scarring and,
even, liver cancer.
Are there different kinds of it?
While Non-alcoholic Fatty Liver (NAFL) is the focus of this post, there are other types of fatty liver disease which include:
- Alcoholic
Fatty Liver which, like its name sounds, is related to alcohol intake.
This form can lead to cirrhosis. It is important to note that alcoholism
can lead to cirrhosis, but normal social use of alcohol can still be a
contributor to fatty liver.
- Non-alcoholic Steatohepatitis (NASH)
is a much more serious form of fatty liver disease than NAFL. If left
untreated, it can permanently scar your liver or lead to death from
liver failure.
- Acute Fatty Liver of Pregnancy often occurs
during the third trimester of pregnancy and can cause symptoms such as
constant nausea and vomiting, pain in the upper right abdomen, fatigue,
and jaundice. Since it can be life threatening if not treated, you need
to talk to your obstetrician about getting screened for it if you are
pregnant and have any of these symptoms. Fortunately, most women
completely recover from it after delivery. [4, 5]
How does it happen?
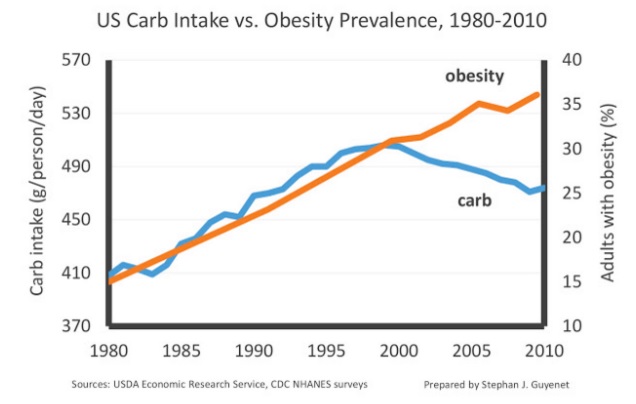
Today,
about a third of Americans are obese, with rates projected to reach 60%
in thirteen states by 2030. Genes that make us more likely to have
obesity or diabetes combined with little exercise and poor diet,
definitely contribute to fatty liver. Then, as the liver has trouble
functioning, other symptoms start to show up, such as reduced energy
levels or muscles which don’t repair as readily, which make it harder to
exercise or prepare healthier foods. It should come as no surprise that
fatty liver is on the rise and this trend doesn’t appear to be changing
anytime soon.
However, many who develop fatty liver are lean and have no apparent health issues. This is why screening is important.
Who is most at risk?
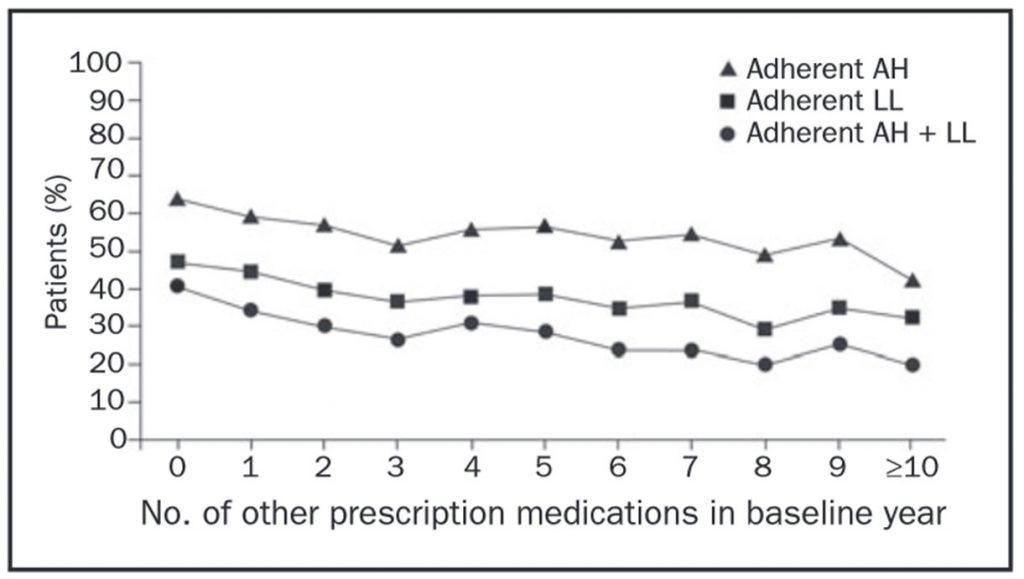
Fatty
liver disease is more common in those who have Type 2 diabetes or who
carry some extra weight. Other factors that have been linked to fatty
liver disease include alcohol use, malnutrition, high cholesterol, high
triglycerides, metabolic syndrome, genetic predisposition, rapid weight
loss, and pregnancy. Medications such as aspirin, acetaminophen
(Tylenol), steroids, tetracycline, tamoxifen, and calcium channel
blockers (blood pressure pills like amlodipine or diltiazem) have also
been linked to this condition.
What are the consequences?
Fatty
liver can lead to early death from liver damage. Among fatal diseases,
it is the only one that has been causing more deaths year after year
since the 1940s.
Those with a fatty liver are also at higher risk
for liver cancer, diabetes, and heart disease. In fact, the most common
cause of death in those with fatty liver is heart disease. [6]
How do I know if I have it?
Get your liver function tested annually.
As
many as 80% of people walking around with fatty liver don’t even know
they have it. A common way someone learns they have fatty liver is that
their doctor finds abnormal liver enzyme levels during an ALT test. Most
blood tests include a metabolic panel, also known as a ‘chem panel’
which includes liver enzymes. ALT, or alanine aminotransferase, is an
enzyme found in your liver. When liver cells are naturally breaking
down, they release some of their contents into your bloodstream. While
some of these enzymes in your bloodstream are perfectly healthy, a liver
inflamed with excess triglycerides or one that is injured causes ALT
scores to creep up.
ALT levels greater than 19 for women and 30
for men are suggestive of fatty liver. Both patients and doctors often
miss this because you can be above this cut off, but still in the normal
range. [7]
Some patients do develop symptoms that bring them to
our clinic. These can include vague pain and discomfort on the upper
right portion of the abdomen or an increase in bloating, gas, or
heartburn. Sometimes patients tell us they have pain in the right
shoulder. While we can see clues that a person has fatty liver disease
from a physical exam, ultrasound. or a liver biopsy, fatty liver is most
often diagnosed when a doctor finds abnormal ALT test results.
Is there hope?
Yes!
Unchecked,
the disease can lead to liver transplant and possible fatality. The
good news is that in the vast majority of cases, fatty liver can be
managed, or even reversed, through a few simple action steps.
Here are the top 10 keys to manage fatty liver disease:
- Stop drinking. If you have fatty liver disease, or are even at risk for it, there is NO safe amount of alcohol.
- Know your ALT level.
If you’re a woman, your ALT should be below 19 and, if you’re a man, it
should be below 30. If your ALT level is higher than that, talk to your
doctor about the possibility of fatty liver. Of course, there are other
causes of your liver enzymes being higher, but in the absence of other
causes, fatty liver is the most likely culprit. If your ALT is high for
no other reason, take the steps below and retest every 3 months.
- Lose weight.
Not everyone with fatty liver is overweight but, for those who are,
losing just 5 to 10 pounds may be enough to radically improve liver
function. Studies have shown that fatty liver responds well to diets
that are low enough in calories to cause 1-1.5 pounds per week of weight
loss. Low carb or low fat can work equally well as long as they are low
in calories but not too low. Rapid weight loss of more than 2 pounds
per week can make things worse.
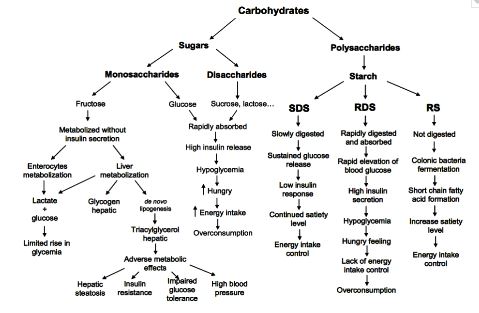
- Manage your blood sugar.
Eating foods high in fiber and lean protein, as well as eating small,
frequent meals, can help heal your liver by balancing your blood sugar
resistance. Fiber has a double benefit for those with fatty liver. It
helps blood sugar and binds with toxins that would otherwise go from
your colon into your liver. The highest sources include white beans,
split peas, lentils, artichokes, broccoli, blackberries, and Brussels
sprouts.
- Avoid fructose. Yes, this does include fresh
fruit. Even though fruit is delicious and is a better choice than candy
or sugary soda, fructose is the type of sugar that is most apt to harm
your liver. [8]
- Limit saturated fat.
Studies have shown that saturated fat can make fatty liver worse, even
when you don’t consume excess calories. [8] If you are eating lower
carb, monounsaturated and polyunsaturated fats are likely the safest for
those with fatty liver. If fatty liver is a concern, limit coconut oil
and leave butter out of your coffee.
- Cut trans fatty acids.
Primarily found in processed foods and baked goods, trans fats can
cause liver damage. Some big sources are fried foods, pie crusts,
margarine, shortening, frosting, pancake mixes, non dairy creamer,
microwave popcorn, animal fat, store bought cookies, biscuits, creamy
frozen drinks, crackers.
- Get enough magnesium. Since
the soil has been farmed out and water is often stripped of its mineral
content, eat foods high in it and consider taking a magnesium
supplement. Surprisingly, magnesium acts as an antioxidant within the
liver. Best food sources include adzuki beans, pumpkin seeds, avocados,
oysters, and spinach. [9, 10]
- Take 400-1200 International Units of Vitamin E every day.
This is above the amount found in foods. Mixed tocopherol versions of
vitamin E are best. Studies of liver biopsies have found this level of
Vitamin E can halt the progression of fatty liver disease within 5
months. [11]
- Use betaine, a naturally occurring substance found in beets.
Also called trimethylglycine, it has been found to lower ALT levels by
40-50% for most people. Using fresh or powdered beet juice is a great
option, as is betaine supplements. [12, 13]
Takeaway Points
Fatty
liver is common and deadly. Thankfully, the pathway back to health is
fairly simple. Subtract alcohol, fructose, and trans fats from your
diet. Then, add some of the nutrients we mentioned earlier. Eating
strategically will give you the energy you need to fuel a healthy
lifestyle. Make sure you talk to your doctor about your ALT level and
encourage your loved ones to do the same.
Even more so than other
parts of your body, your liver can regenerate if you give it a chance.
As always, learn about your own health, and never give up!

[1]
Browning J.D., Szczepaniak L.S., Dobbins R., et al. “Prevalence of
Hepatic Steatosis in an Urban Population in the United States: Impact of
Ethnicity.”
Hepatology 40.6 (2004):1387–1395.
[2] Lazo M., Clark J.M. “The Epidemiology of Nonalcoholic Fatty Liver Disease: a Global Perspective.”
Seminars in Liver Disease 28.4 (2008): 339–350.
[3]
http://www.medscape.com/viewarticle/584214_8
[4] Healthline Editorial Team.
What are the Types of Fatty Liver? Healthline, 2 Oct. 2015. Web. 27 Mar. 2016. <
http://www.healthline.com/health/fatty-liver#Types4>
[5] American Liver Foundation.
Nonalcoholic Fatty Liver Disease. American Liver Foundation. 14 Jan. 2015. Web. 27 Mar. 2016. <
http://www.liverfoundation.org/abouttheliver/info/nafld/>
[6] The Lancet.
The Lancet Liver Campaign. The Lancet, Jul. 2015. Web. 27 Mar. 2016. <
http://www.thelancet.com/campaigns/liver?utm_source=email&utm_medium=Li verEM1&utm_campaign=liver>
[7] Paschos, P., Paletas, K. “Non alcoholic Fatty Liver Disease and Metabolic Syndrome.”
Hippokratica 13.1 (2009): 9-19. <
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2633261/>
[8] Sullivan, S. “Implications of Diet on Nonalcoholic Fatty Liver Disease.”
Current Opinion in Gastroenterology 26.2 (2010): 160-164. <
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3732059/>
[9]
Nadler J.L., Buchanan T., Natarajan R., et al. “Magnesium Deficiency
Produces Insulin Resistance and Increased Thromboxane Synthesis.”
Hypertension 21 (1993): 1013-1019.
[10] Afanas’ev I.B., Suslova T.B., Cheremisina Z.P., et al. “Study of Antioxidant Properties of Metal Aspartates.”
Analyst 120 (1995): 850-862.
[11]
Parola M., Muraca R., Dianzani I., et al. “Vitamin E Dietary
Supplementation Inhibits Transforming Growth Factor Beta-1 Gene
Expression in Rat Liver.”
Federation of European Biochemical Societies Letters 308 (1992): 267-270.
[12]
Abdelmalek M.F., Angulo P., Jorgensen R.A., et al. “Betaine, a
Promising New Agent for Patients with Nonalcoholic Steatohepatitis:
Results of a Pilot Study.”
American Journal of Gastroenterology 96 (2001): 2711- 2717.
[13] Mukherjee, S. “Betaine and Nonalcoholic Steatohepatitis: Back to the Future?”
World Journal of Gastroenterology 17.32 (2011): 3663–3664.
Dr.
Alan Christianson is an Arizona-based Naturopathic Physician who helps
people overcome adrenal and thyroid disorders and achieve lasting fat
loss. He authored the New York Times' bestselling Adrenal Reset Diet,
and The Complete Idiot’s Guide to Thyroid Disease. Dr. Christianson is
the founding physician behind Integrative Health.
Dr. Christianson can be reached at
www.MyIntegrativeHealth.com, www.DrChristianson.com and 480-657-0003.














 What is it?
What is it?