
You know how people talk about being thankful for major diseases because of some lesson they learned? Have you ever heard that and thought, “Yeah, right, I’d just as soon skip that lesson.” Here is one I’m glad I did learn, albeit the hard way.
I learned how to take pills. I planned a list of pre- and post-surgical supplements to help me repair and get the general anesthesia out of my brain. Since there were so many surgeries back to back, I didn’t want to miss a single pill. Most pills don’t work because we don’t take them regularly.
I’ve never taken large numbers of pills before and I really didn’t have a system. So, I read a few dozen papers on the topic of ‘medication adherence’ and built a system.
It amazed me what a problem this was. Would you believe that people who were told if they missed their pills that they would die of a stroke still could not take it regularly? The graph below represents how successful adults were with taking medication to prevent the risk of a second stroke. By two years out, most have quit their treatment. [1]

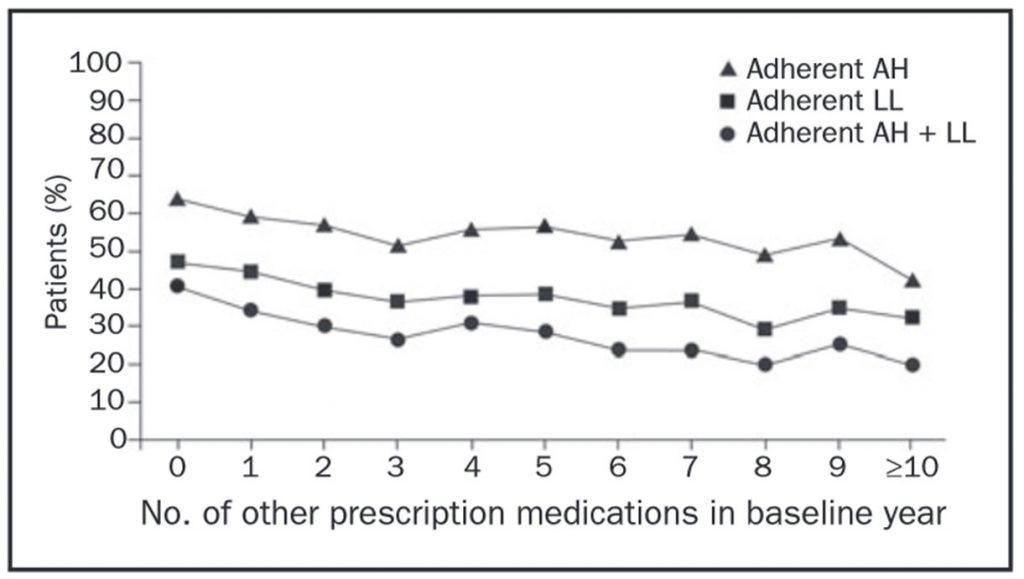
Some things that make it worse include how many pills you take and how often you take them. The graph below shows how adding pills lowers the odds of people regularly taking two different medications based on how many other pills they were taking. The line with the circles shows that only about 30% took both pills regularly, with regularly being defined as 80% of the time. [2]
How often you take pills can also be a factor. More than once daily is much harder than once daily; four times daily is the hardest of all. [3]

How can you do better? Create a weekly pill ritual for yourself. Since we are all creatures of habit, good and bad, you may as well use this fact to your advantage. Here is my ritual.
I set aside 15 minutes each Sunday afternoon at 4 pm. Another block can work but the idea is you want a period of time in your week in which nothing else important will intrude and you’re not pressured with other tasks or obligations.
Set this up as a recurrent event so it happens each week even if you don’t think about it.
Here is what to do with that 15 minutes:
1. Write – I created a list of non prescription and prescription pills I was taking. Include dosage, potency, how often to take, whether to take with or without food, how long to stay on, and what are they for. Below is a table with sample entries.

2. Review – Once the list was written, I did not have to rewrite it each week but I do review it and update it.
3. Refill – I check my supplies and reorder anything that was going to run out within the next two weeks or set a reminder to pick it up from my office the following day.
4. Restock – I refill my weekly pill box. I’ve got one that is just big enough for each day’s pills and allows me to take a few days worth of pills out separately so I don’t have to bring the whole box when I travel.

An easy way is to set the bottles all on one side of it and move them one at a time to the other side as you place the pills in the bins. Sometimes they look the same and you can’t tell otherwise which ones you already put in yet and which ones you did not.
5. Remind – I do a pretty good job at my breakfast pills. If I don’t eat at home on a given evening, I’ll take the evening’s pills in my pocket or in a snack-sized bag. If you are not yet in a rhythm, find a reminder system and make sure it is set for the week. Lots of apps are available that do this well.
Look ahead and make sure your alarms are all set for the right times. Revise if your current system is not working for some reason.
If you really can’t remember, get a pill box with a built-in reminder.

Once you get this rhythm down you will find pills are no longer a source of stress. You might be amazed how much benefit you can get from simple steps when you are able to do them consistently.
Along with recovering faster than expected from surgery, I had a bonus win. My stylist told me my hair has gotten much thicker since I started this habit!
[1] Brown M.T., Bussell J.K. Medication adherence: WHO cares? Mayo Clin. Proc. 2011; 86:304–314.
[2] Brown M.T., Bussell J.K. Medication adherence: WHO cares? Mayo Clin. Proc. 2011; 86:304–314.
[3] Brown M.T., Bussell J.K. Medication adherence: WHO cares? Mayo Clin. Proc. 2011; 86:304–314.
 (c) 2015- Integrative Health Care, PC
(c) 2015- Integrative Health Care, PCWould you like to use this article? You may as long as you use the following information along with the article:
Dr. Alan Christianson is an Arizona-based Naturopathic Physician who helps people overcome adrenal and thyroid disorders and achieve lasting fat loss. He authored the New York Times' bestselling Adrenal Reset Diet, and The Complete Idiot’s Guide to Thyroid Disease. Dr. Christianson is the founding physician behind Integrative Health.
Dr. Christianson can be reached at www.MyIntegrativeHealth.com, www.DrChristianson.com and 480-657-0003.












